Phenotypic Detection and Antibiotic Susceptibility Pattern of Extended-Spectrum β-Lactamase-Producing Uropathogenic E. coli Isolated in Sana'a City, Yemen
Main Article Content
Abstract
Background: Urinary tract infections pose a significant public health challenge in Yemen, exacerbated by the emergence of extended spectrum -lactamase-producing uropathogenic E. coli. This study aimed to determine the prevalence and antimicrobial susceptibility profile of extended-spectrum -lactamase-producing uropathogenic E. coli in Sana’a City.
Methods: A cross-sectional study collected 359 urine samples from two major hospitals in Sana’a. Uropathogenic E. coli isolates were identified using standard methods, and ESBL production was confirmed phenotypically using the double-disk synergy test. Antimicrobial susceptibility was determined via Kirby-Bauer disk diffusion
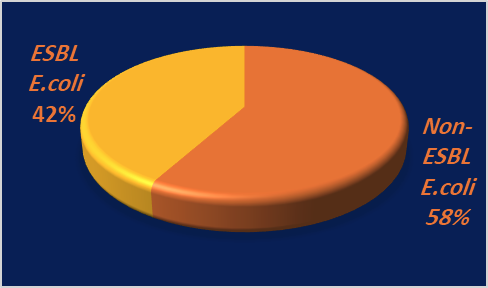
Results: Of the samples, 155 (43.1%) were positive for uropathogenic E. coli, with 41.9% (65/155) confirmed as ESBL producers. These isolates exhibited high resistance to ampicillin, cephalosporins, and fluoroquinolones. Amikacin and meropenem remained the most effective antibiotics. Extended-spectrum -lactamase-producing uropathogenic E. coli infections showed significant associations with comorbidities including diabetes, heart disease, and urinary tract deformities (p < 0.05).
Conclusion: The high prevalence of multidrug-resistant extended spectrum -lactamase-producing uropathogenic E. coli among Yemeni urinary tract infection in Sana’a city underscores the urgent need for routine susceptibility testing and antimicrobial stewardship programs to guide treatment and preserve effective antibiotics.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
- P.Katongole, F.Nalubega, N. Florence, B. Asiimwe , I. Andia , Biofilm formation, antimicrobial susceptibility and virulence genes of Uropathogenic Escherichia coli isolated from clinical isolates in Uganda. MC Infectious Diseases, 20(453)( 2020).p:1-6. https://doi.org/10.1186/s12879-020-05186-1.
- A.S., Emekekwue, M.C., Ugwu, C.P., Ejikeugwu, D.C., Nwobodo, N.T., Ujam, U.M., Okezie, I.R. Iroha, and C. O. Esimone, Prevalence and antibiogram of ESBL-positive uropathogenic Escherichia coli in pregnant women in Onitsha Metropolis, Nigeria. International Journal of Pharmaceutical and Phytopharmacological Research, 12(6)(2022), pp.8–18. . https://doi.org/10.51847/x5e62APEMI
- F.S., Mitu, M.A., Al Maruf , A., Mahanty , A.N., Huda, S.A., Khan, M.M. Rahman, Prevalence of extended spectrum beta-lactamase (ESBL) and AmpC beta-lactamase producing bacteria in urinary tract infection patients in Bangladesh. Malays..15(3) (2019), 204–212. DOI: http://dx.doi.org/10.21161/mjm.180193
- M. H. Omar, A.M. Kilale, H. K.Rashid, E. R. Mwakapeje, I. M.e Onoka, A.A. Gimbi, Prevalence and risk factors for extended-spectrum βlactamase producing antimicrobial-resistant E. coli in urinary tract infections among inpatients in the tertiary hospitals in Zanzibar (Tanzania): a prospective cross-sectional study. PAMJ - 47(193) (2024). P .1-11. DOI: 10.11604/pamj.2024.47.193.37920
- M.K., Aworh, J., Kwaga, E., Okolocha, N. Mba, and S. Thakur, Prevalence and risk factors for multidrug resistant Escherichia coli among poultry workers in the Federal Capital Territory, Abuja, Nigeria. PLoS ONE, 14(11)(2019),1-15. https://doi.org/10.1371/journal.pone.0225379.
- S., Nasher, S., Alsharapy, A. Al-Madhagi, and F. Zakham, 'Epidemiology of extended-spectrum β-lactamase producing Escherichia coli from hospital settings in Yemen', Journal of Infection in Developing Countries, 12(11)(2018), pp. 953–959. doi:10.3855/jidc.10560
- M.B. Jalil, and M.Y. Al Atbee, The prevalence of multiple drug resistance Escherichia coli and Klebsiella pneumoniae isolated from patients with urinary tract infections. .Jcla. 36 (9)(2022) e24619. https://doi.org/10.1002/jcla.24619
- S., Teferi, Z., Sahlemariam, M., Mekonnen, R., Tamrat, T., Bekana, Y.Adisu, and T. Darge, Uropathogenic bacterial profile and antibiotic susceptibility pattern of isolates among gynecological cases admitted to Jimma Medical Center, South West Ethiopia. Scientific Reports, 13 7078 (2023) . https://doi.org/10.1038/s41598-023-34048-4
- S.M. Hasan, and K.S. Ibrahim, Molecular Characterization of Extended Spectrum β-Lactamase (ESBL) and Virulence Gene-Factors in Uropathogenic Escherichia coli (UPEC) in Children in Duhok City, Kurdistan Region, Iraq’, Antibiotics, 11(9) (2022). 1246. doi:10.3390/antibiotics11091246.
- M., Matsukawa, M., Igarashi, H., Watanabe, L., Qin, M., Ohnishi, Terajima, J., Iyoda, S., Morita-Ishihara, T., Tateda, K., Ishii, Y., Saga, T., K. Aoki, and R.A., Bonomo, Epidemiology and genotypic characterisation of dissemination patterns of uropathogenic Escherichia coli in a community. Epidemiology and Infection, 147(2019)., e148. https://doi.org/10.1017/S0950268819000426
- Clinical Laboratory Standards Institute (CLSI), Performance standard for antimicrobial susceptibility testing, CLSI M100. 4(10) 2020.
- B.M., Mahdi, H.B. Khudhur, and M.M., Abdul-Hussein, Bacterial isolates of urine and their susceptibility to antimicrobials. Macedonian Journal of Medical Sciences, 8(A) (2020), pp.84–88. https://doi.org/10.3889/oamjms.2020.4086
- B., Behera, M., Debbarma, B., Rout, P., Baral, S., Das, L. Jena, and R., Panigrahy, Prevalence of ESBL producing bacteria in community-acquired UTI from Eastern part of India. Journal of Pure and Applied Microbiology, 16(3)(2022), pp.1682–1688. https://doi.org/10.22207/JPAM.16.3.07
- S., Moubayed, J., Ghazzawi, R. Mitri, and S. Khalife, Recent data characterizing the prevalence and resistance patterns of FimH-producing uropathogenic Escherichia coli isolated from patients with urinary tract infections in North Lebanon. Archives of Clinical Infectious Diseases, 18(4)( 2023), e135782. https://doi.org/10.5812/archcid-135782
- S.A.A., Alghamdi, S.S., Mir, F.S., Alghamdi, M.A.M.A., Al Banghali, S.S.R.Almalki, and S.S., Rajab, Evaluation of Extended-Spectrum Beta-Lactamase Resistance in Uropathogenic Escherichia coli Isolates from Urinary Tract Infection Patients in Al-Baha, Saudi Arabia. Microorganisms, 11(12)( 2023), 2820. https://doi.org/10.3390/microorganisms11122820
- P., Jia, Y. Zhu, X. Li, High prevalence of extended-spectrum beta-lactamases in Escherichia coli strains collected from strictly defined community-acquired urinary tract infections in adults in China: a multicenter prospective clinical microbiological and molecular study', Frontiers in Microbiology, 12 (2021) 663033. DOI: 10.3389/fmicb.2021.663033
- S.T., Ahn, H.S., Lee, D.E., Han, D.H., Lee, J.W., Kim, M.G., Park, H.S.,Park, D.G. Moon, and M.M., Oh, What are the risk factors for recurrent UTI with repeated ESBL-producing Enterobacteriaceae? A retrospective cohort study. Journal of Infection and Chemotherapy, 29(1)( 2023), pp.72–77. https://doi.org/10.1016/j .jiac.2022.09.013
- J.P. Camargo-Mendoza, and D.E., Ariza-Rodríguez, Risk factors for health care-associated infections by ESBL-producing germs in an intensive care unit of a public hospital in Bogotá D.C., Colombia. Revista de la Facultad de Medicina,70(4)(2022)e92755. https://doi.org/10.15446/revfacmed.v70n4.92755
- P., Vachvanichsanong, E.B. McNeil, and P., Dissaneewate, Extended-spectrum beta-lactamase Escherichia coli and Klebsiella pneumoniae urinary tract infections. Cambridge University Press. 17:149:e12 (2020) DOI: 10.1017/S0950268820003015
- Z., Asmare, M., Erkihun, W. Abebe, and E. Tamrat, Antimicrobial resistance and ESBL production in uropathogenic Escherichia coli: a systematic review and meta-analysis in Ethiopia', JAC-Antimicrobial Resistance, 6(3)( 2024.), dlae068. DOI: 10.1093/jacamr/dlae068
- E. S. Khater, and H. w. Sherif, Association between virulence factors and antibiotic resistance in E.coli isolated from urinary tract infection patient in Banha University Hospitals, Egypt. Merit Research Journal of Microbiology and Biological Sciences. 9(1)(2021) pp. 001-008, DOI: 10.5281/zenodo.4661556.