The Association Between Antibiotic Resistance and Biofilm Production in Klebsiella pneumoniae Isolated from Urinary Tract Infections.
Main Article Content
Abstract
Background and aims This research investigates the link between biofilm formation and antibiotic resistance among Klebsiella pneumoniae bacteria in Sana'a city, Yemen, a common cause of hospital-acquired infections and community-acquired infections.
Methods: A 6-month study investigated 300 urinary tract infections samples, with 241 culture-positive. Standard methods were used for isolation and identification, including biofilm production and antibiogram susceptibility patterns of Klebsiella pneumoniae.
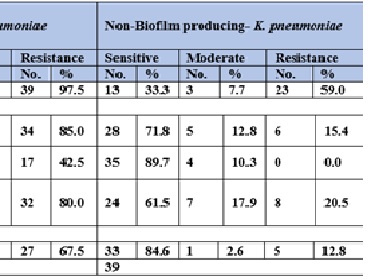
Results: The study reveals that penicillin resistance is linked to Klebsiella pneumoniae's ability to form biofilms. Ampicillin-resistant isolates formed biofilms 97.5% of the time, while non-biofilm-producing isolates had a lower rate of resistance. Carbapenem group resistance was also significant, with Meropenem-resistant isolates forming biofilms 42.5% of the time. Cephalosporin resistance ranged from 80-95% for Biofilm-Forming Isolates, while Quinolones resistance ranged from 65-82%. Aminoglycoside resistance was also significant, with gentamicin and amikacin resistance rates being 42.5% and 42.5%, respectively. These findings highlight the importance of understanding the phenotypes of Klebsiella pneumoniae in forming biofilms.
Conclusion: The study found a strong correlation between the biofilm production of Klebsiella pneumoniae and antibiotic resistance, with quinolones and cephalosporins being the least active, while carbapenems and aminoglycosides showed slight sensitivity.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.